Knowledge Translation
Our team synthesises, disseminates, reviews and exchanges evidence based ethically-sound knowledge to help improve the health and well being of those who suffer from all forms of allergies.

WAO
Time to ACT-UP: Update on precautionary allergen labelling (PAL)
WAO
Time to ACT-UP: Update on precautionary allergen labelling (PAL)
September 25, 2024
Background: Precautionary Allergen ("may contain") Labelling (PAL) is used by industry to communicate potential risk to food-allergic individuals posed by unintended allergen presence (UAP). In 2014, the World Allergy Organization (WAO) highlighted that PAL use was increasing, but often applied inconsistently and without regulation - which reduces its usefulness to consumers with food allergy and those purchasing food for them. WAO proposed the need for a regulated, international framework to underpin application of PAL. In 2019, the World Health Organization (WHO) and the Food and Agriculture Organization (FAO) of the United Nations convened an expert consultation to address the issue of PAL, the outputs of which are now being considered by the Codex Committee on Food Labelling (CCFL).
Objectives: To summarise the latest data to inform the application of PAL in a more systematic way, for implementation into global food standards.
Methods: A non-systematic review of issues surrounding precautionary labelling and food allergens in pre-packaged products.
Results: Approximately, 100 countries around the world have legislation on the declaration of allergenic ingredients. Just a few have legislation on UAP. Given the risks that UAP entails, non-regulated PAL creates inconvenience in real life due to its unequal, difficult interpretation by patients. The attempts made so far to rationalize PAL present lights and shadows.
Conclusions: At a time when CCFL is considering the results of the FAO/WHO Expert Consultation 2020-2023, we summarise the prospects to develop an effective and homogeneous legislation at a global level, and the areas of uncertainty that might hinder international agreement on a regulated framework for PAL of food allergens.
Objectives: To summarise the latest data to inform the application of PAL in a more systematic way, for implementation into global food standards.
Methods: A non-systematic review of issues surrounding precautionary labelling and food allergens in pre-packaged products.
Results: Approximately, 100 countries around the world have legislation on the declaration of allergenic ingredients. Just a few have legislation on UAP. Given the risks that UAP entails, non-regulated PAL creates inconvenience in real life due to its unequal, difficult interpretation by patients. The attempts made so far to rationalize PAL present lights and shadows.
Conclusions: At a time when CCFL is considering the results of the FAO/WHO Expert Consultation 2020-2023, we summarise the prospects to develop an effective and homogeneous legislation at a global level, and the areas of uncertainty that might hinder international agreement on a regulated framework for PAL of food allergens.
World Allergy Organ J . 2024 Sep 25;17(10):100972. doi: 10.1016/j.waojou.2024.100972.

The Dermatology Digest
The Itch Factor Unpacking the New AAAAI/ACAAI Joint Task Force Guidelines on AD
The Dermatology Digest
The Itch Factor Unpacking the New AAAAI/ACAAI Joint Task Force Guidelines on AD
March 14, 2024
Following a prolonged period of little progress, there has been a surge in the approval of new treatments for atopic dermatitis (AD), with numerous others in different stages of development. For healthcare professionals treating AD, the abundance of options can be daunting, posing challenges to effectively incorporating these new therapies into patient care. The American Academy of Allergy, Asthma & Immunology (AAAAI) and the American College of Allergy, Asthma & Immunology (ACAAI) Joint Task Force (JTF) recently released updated guidelines for AD management, encompassing several of the latest medications and addressing five crucial questions related to AD management:
The Dermatology Digest
JACI In Practice
Impacts of Determinants of Health on Atopic Dermatitis, Pathways Towards Solutions, and Unique Considerations for Rural and Remote North American Indigenous Populations
JACI In Practice
Impacts of Determinants of Health on Atopic Dermatitis, Pathways Towards Solutions, and Unique Considerations for Rural and Remote North American Indigenous Populations
November 24, 2023
Disparities in environmental and social determinants of health (DOH) are associated with morbidity in atopic dermatitis (AD). The socioecological model (SEM) is a framework that can be applied to better understand how DOH impacts patients with AD. We include a case scenario of a remote Indigenous patient reflective of real-world situations of living with AD and examine relevant impact, gaps in knowledge, and further research needs. This review highlights a variety of social and environmental exposures as important DOH which must be addressed to achieve optimal management in AD. The "Rainbow model” is a modified framework to help illustrate how complex environmental and social forces impact both AD presentation and therapeutic success. However, practical applications and outcome metrics for health promotion are limited.1 An inter- and transdisciplinary approach is paramount to address the complex challenges associated with AD care, as well as multistakeholder approach integrating culturally-competent equitable health frameworks. This review underscores the importance of expanding the focus of AD management beyond basic science and clinical trials to recognize and address health disparities and to promote optimal health and well-being in patients with AD, and contributes a working approach to mapping the complex interventions and patient-oriented research needed using a focus on remote North American Indigenous patients affected by AD.
In Press

BMJ
A guide and pragmatic considerations for applying GRADE to network meta-analysis
BMJ
A guide and pragmatic considerations for applying GRADE to network meta-analysis
June 27, 2023
Assessing the certainty of evidence from network meta-analyses using the GRADE (grading of recommendations, assessment, development, and evaluations) approach requires not only a thorough understanding of the methods but also substantial workload for raters. This article describes how implementing practical strategies (including rule setting and automation) can facilitate efficient application of the GRADE approach to rating certainty of evidence in network meta-analyses while maintaining rigor.
BMJ 2023;381:e074495

JACI In Practice
Skin antiseptics for atopic dermatitis: dissecting facts from fiction
JACI In Practice
Skin antiseptics for atopic dermatitis: dissecting facts from fiction
January 22, 2023
Staphylococcus aureus (S. aureus) is a known trigger and cause of infectious complications in atopic dermatitis (AD). Various antiseptics have been used in an attempt to decrease the burden of S. aureus in AD. In this Commentary, we present the evidence for and against some of the commonly-used antiseptics in clinical and research settings. These agents remain attractive as an adjunct therapy for AD due to their relative low cost and potential benefits of reducing S. aureus. Though a number of studies have evaluated the use of dilute bleach, its mechanisms remain controversial. A higher concentration of bleach than the commonly-used 0.005% is likely needed for its anti-S. aureus effect. Silver-coated textiles have demonstrated anti-S. aureus effects in various studies, however, their efficacy and side effects in AD remain to be confirmed. Other antiseptics including chlorhexidine, triclosan and triclocarban are also discussed. Variables that may affect the outcomes of these studies include length of use, concurrent application of moisturizers and anti-inflammatory medications.
Ong, PY, Boguniewicz, J, Chu DK. The Journal of Allergy and Clinical Immunology: In Practice, In Press

Canadian Allergy & Immunology Today
Atopic Dermatitis and Canadian Indigenous Peoples: Burdens, Barriers, and Potential for Solutions
Canadian Allergy & Immunology Today
Atopic Dermatitis and Canadian Indigenous Peoples: Burdens, Barriers, and Potential for Solutions
December 1, 2022
Atopic dermatitis (AD) is the most common chronic inflammatory skin disease worldwide. AD begins before age five in 90% of cases and is associated with the development of comorbid conditions such as infections, environmental allergies, food allergies, asthma, anxiety/depression, and abnormalities in sleep, growth, and development. While personal experience suggests that Canadian Indigenous peoples, including children and youth, are facing burdens associated with AD, formal research studies addressing the impact of AD and skin disease in general on Canadian Indigenous peoples are lacking. Canadian Indigenous* account for approximately 5% of the Canadian population. Although Canadian Indigenous vary widely in geography, culture, language, and beliefs, they face common health disparities embedded in complex historical and social contexts related to factors such as colonization, intergenerational trauma from residential schools and institutionalization, racial segregation in the form of reservations, systemic racism, and being subjected to policies such as the ‘Indian Act’. This article reviews the burdens and barriers of AD in Canadian Indigenous by examining the literature, experiences of health care practitioners (HCPs), and media reports followed by proposing potential solutions to address such disparities.
Can Allergy Immunol Today. 2022 Dec. 1;2(3):26–30.

Canadian Medical Association Journal (CMAJ)
How to manage atopic dermatitis in infants
Canadian Medical Association Journal (CMAJ)
How to manage atopic dermatitis in infants
November 7, 2022
Atopic dermatitis affects an 10-20% of Canadian infants and negatively impacts patient and caregiver quality of life in many ways. Despite this, optimal treatment is challenging, with caregivers often leaving clinical encounters unequipped to gain self-efficacy and clinicians uncertain of which treatments to promote or demote. There is also increasing evidence for addressing comorbidity in atopic dermatitis, particularly its role in promoting the development of food allergy and the importance, for infants, of timing of food allergen introduction in food allergy prevention. To address these issues, we summarize five key messages for general and specialist care providers as well as caregivers to better understand how to manage atopic dermatitis.
CMAJ November 07, 2022 194 (43) E1485

JAMA Pediatrics
What Parents Should Know About Atopic Dermatitis
JAMA Pediatrics
What Parents Should Know About Atopic Dermatitis
September 26, 2022
Atopic dermatitis (AD) is a chronic skin condition that results in dry, itchy, and red skin.
More than 1 in 10 children are affected. It is caused by dysfunction of the skin barrier and an imbalanced immune system. Children with AD are often described as having sensitive skin.
More than 1 in 10 children are affected. It is caused by dysfunction of the skin barrier and an imbalanced immune system. Children with AD are often described as having sensitive skin.
JAMA Pediatr. doi:10.1001/jamapediatrics.2022.3109
JACI In Practice
Boxed warnings and off-label use of allergy medications: risks, benefits, and shared decision making
JACI In Practice
Boxed warnings and off-label use of allergy medications: risks, benefits, and shared decision making
September 6, 2022
The Food and Drug Administration (FDA) is tasked with evaluating the efficacy and safety of a drug. Despite having a regimented appraisal process in place, safety evidence can emerge during clinical trials as well as from observations and studies conducted after the drug has been on the market that might require a boxed warning. The boxed warning is the most severe warning that the FDA can give to an approved drug. It is commonly referred to as a Black Box Warning as it is outlined in the package insert by a thick black box to garner the attention of prescribers and patients. There are currently over 400 medications that have boxed warnings and the information addressing major risks associated with a particular drug may, appropriately or inappropriately, influence patient and clinician decision making. Healthcare professionals must use the best evidence and clinical judgment in determining whether to prescribe medications with these warnings. Use of an approved drug at dosages or for indications other than what it was originally licensed for is referred to as “off-label” and is legal, commonplace, and may be evidence-based. All drugs may expose patients to possible harm, so prescribers have an obligation to discuss the best available evidence regarding benefits and harms so that patients can participate in shared decision-making.
The Journal of Allergy and Clinical Immunology: In Practice (2022), doi: https://doi.org/10.1016/ j.jaip.2022.08.033.
World Allergy Organization
Diagnosis and Rationale for Action against Cow's Milk Allergy (DRACMA) Guidelines update - III - Cow's milk allergens and mechanisms triggering immune activation
World Allergy Organization
Diagnosis and Rationale for Action against Cow's Milk Allergy (DRACMA) Guidelines update - III - Cow's milk allergens and mechanisms triggering immune activation
September 1, 2022
The immunopathogenesis of cow's milk protein allergy (CMPA) is based on different mechanisms related to immune recognition of protein epitopes, which are affected by industrial processing.
Purpose
The purpose of this WAO DRACMA paper is to: (i) give a comprehensive overview of milk protein allergens, (ii) to review their immunogenicity and allergenicity in the context of industrial processing, and (iii) to review the milk-related immune mechanisms triggering IgE-mediated immediate type hypersensitivity reactions, mixed reactions and non-IgE mediated hypersensitivities.
Results
The main cow’s milk allergens – α-lactalbumin, β-lactoglobulin, serum albumin, caseins, bovine serum albumins, and others – may determine allergic reactions through a range of mechanisms. All marketed milk and milk products have undergone industrial processing that involves heating, filtration, and defatting. Milk processing results in structural changes of immunomodulatory proteins, leads to a loss of lipophilic compounds in the matrix, and hence to a higher allergenicity of industrially processed milk products. Thereby, the tolerogenic capacity of raw farm milk, associated with the whey proteins α-lactalbumin and β-lactoglobulin and their lipophilic ligands, is lost.
Conclusion
The spectrum of immunopathogenic mechanisms underlying cow's milk allergy (CMA) is wide. Unprocessed, fresh cow's milk, like human breast milk, contains various tolerogenic factors that are impaired by industrial processing. Further studies focusing on the immunological consequences of milk processing are warranted to understand on a molecular basis to what extent processing procedures make single milk compounds into allergens.
Purpose
The purpose of this WAO DRACMA paper is to: (i) give a comprehensive overview of milk protein allergens, (ii) to review their immunogenicity and allergenicity in the context of industrial processing, and (iii) to review the milk-related immune mechanisms triggering IgE-mediated immediate type hypersensitivity reactions, mixed reactions and non-IgE mediated hypersensitivities.
Results
The main cow’s milk allergens – α-lactalbumin, β-lactoglobulin, serum albumin, caseins, bovine serum albumins, and others – may determine allergic reactions through a range of mechanisms. All marketed milk and milk products have undergone industrial processing that involves heating, filtration, and defatting. Milk processing results in structural changes of immunomodulatory proteins, leads to a loss of lipophilic compounds in the matrix, and hence to a higher allergenicity of industrially processed milk products. Thereby, the tolerogenic capacity of raw farm milk, associated with the whey proteins α-lactalbumin and β-lactoglobulin and their lipophilic ligands, is lost.
Conclusion
The spectrum of immunopathogenic mechanisms underlying cow's milk allergy (CMA) is wide. Unprocessed, fresh cow's milk, like human breast milk, contains various tolerogenic factors that are impaired by industrial processing. Further studies focusing on the immunological consequences of milk processing are warranted to understand on a molecular basis to what extent processing procedures make single milk compounds into allergens.
World Allergy Organization Journal Volume 15, Issue 9, September 2022, 100668
Trustworthy Patient-Centered Guidelines: Insights From Atopic Dermatitis and a Proposal for the Future
Trustworthy Patient-Centered Guidelines: Insights From Atopic Dermatitis and a Proposal for the Future
July 7, 2022
Not all clinical practice guidelines are trustworthy. A proliferation of guidelines, many with suboptimal rigor and transparency, led the Institute of Medicine to create standards defining objective and consistent guideline development processes. Trustworthy guidelines optimize care by issuing systematically developed statements to assist practitioner and patient decisions addressing optimal health care for specific clinical circumstances. To be trustworthy, guidelines should follow systematic and rigorous development processes, apply the principles of evidence-based medicine, and place patient and caregiver values and preferences as central to optimal decision making.
The Journal of Allergy and Clinical Immunology: In Practice, https://doi.org/10.1016/j.jaip.2022.06.017

JACI In Practice
Translating Evidence to Optimize Patient Care Using GRADE
JACI In Practice
Translating Evidence to Optimize Patient Care Using GRADE
December 1, 2021
Optimal evidence-based clinical practice requires systematic summaries of the best available evidence, including ratings of the quality of that evidence, and is facilitated by the availability of trustworthy guidelines. In this review, we describe the Grading of Recommendations, Assessment, Development, and Evaluation (GRADE) approach to rating quality of evidence and moving from evidence to recommendations using examples from allergy-immunology. GRADE focuses on systematic summaries of the best evidence, systematic reviews and trustworthy guidelines, and emphasizes a structured approach to determining quality (certainty) of bodies of evidence, absolute magnitude of effects of desirable and undesirable consequences (benefits and harms), and use of evidence to develop clinical recommendations. Adopted by over 110 organizations worldwide, including the American Academy of Allergy, Asthma, and Immunology/American College of Allergy, Asthma, and Immunology Joint Task Force on Practice Parameters, GRADE is foundational to the optimal interpretation of research evidence and its application in clinical practice. This review supports the clinician's ability to find and use the information in GRADE guidelines to help care for patients in the clinic.
The Journal of Allergy and Clinical Immunology: In Practice, Volume 9, Issue 12, 2021, Pages 4221-4230
Pediatric Allergy and Immunology
Method’s corner: Allergist’s guide to network meta-analysis
Pediatric Allergy and Immunology
Method’s corner: Allergist’s guide to network meta-analysis
July 29, 2021
Network meta-analyses (NMAs) simultaneously estimate the effects of multiple possible treatment options for a given clinical presentation. For allergists to benefit optimally from NMAs, they must understand the process and be able to interpret the results. Through a worked example published in Pediatric Allergy and Immunology, we summarize how to identify credible NMAs and interpret them with a focus on recent innovations in the GRADE approach (Grading of Recommendations Assessment, Development, and Evaluation). NMAs build on traditional systematic reviews and meta-analyses that consider only direct paired comparisons by including indirect evidence, thus allowing the simultaneous assessment of the relative effect of all pairs of competing alternatives. Our framework informs clinicians of how to identify credible NMAs and address the certainty of the evidence. Trustworthy NMAs fill a critical gap in providing key inferences using direct and indirect evidence to inform clinical decision making when faced with more than two competing courses of treatment options. This document will help allergists to identify trustworthy NMAs to enhance patient care.
Pediatr Allergy Immunol. 2021; 33:e13609.

Lancet Respiratory Medicine
Use of facemasks during the COVID-19 pandemic
Lancet Respiratory Medicine
Use of facemasks during the COVID-19 pandemic
August 3, 2020
As of July 26, 2020, severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) has infected more than 16 000 000 individuals worldwide and caused over 600 000 deaths from COVID-19. Despite advances in pharmacological treatment and early vaccine development, reducing transmission of the virus with the use of facemasks (referring to medical or surgical masks, N-95 and similar respirators, cloth masks, and bandannas) by health-care workers and the public alike remains a hotly debated topic due to politicisation of discourse and decision making.
Annals of Internal Medicine
Rethinking Oxygen Therapy for Hospitalized Patients
Annals of Internal Medicine
Rethinking Oxygen Therapy for Hospitalized Patients
September 17, 2019
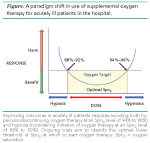
Oxygen therapy has been a critical life-saving measure since its first use for pneumonia in the 19th century. With its widespread use in contemporary medicine came the notion that supplemental oxygen is harmless, and that it may even be beneficial in nonhypoxemic patients. Over time, this conviction has become ingrained in clinical practice and the medical training of health care providers. Indeed, the classic mantra taught for any acutely ill patient is, “ABC IV O2 Monitor.”
Ann Intern Med.2019;171:HO2-HO3.

The Intern at Work
Podcast for Internal Medicine - Penicillin allergy “Rash Decisions”
The Intern at Work
Podcast for Internal Medicine - Penicillin allergy “Rash Decisions”
April 14, 2019
Penicillin Allergy
Ask a Fellow: Rash Decisions - Penicillin Allergy
Guest Fellows: Dr. Derek Chu (Clinical Allergy and Immunology), Dr. David McCullagh (Infectious Diseases)
Infographic by: Rachel Ahle (Physician Assistant Student)
Ask a Fellow: Rash Decisions - Penicillin Allergy
Guest Fellows: Dr. Derek Chu (Clinical Allergy and Immunology), Dr. David McCullagh (Infectious Diseases)
Infographic by: Rachel Ahle (Physician Assistant Student)
AAAAI
Food Labels: Read It Before You Eat It!
AAAAI
Food Labels: Read It Before You Eat It!
January 16, 2019
For people with food allergies, food allergen avoidance is a critical part of preventing allergic reactions. Understanding how to read a food label is necessary to effectively avoid any food to which one might be allergic.
Reading a food label for allergens is different from what you might be used to. It is more than just looking at the carbs, protein, salt and calorie count. Instead, for food allergies, the ingredient list and any warning labels are the most important. However, packaged and processed foods often contain many ingredients and sometimes they are not labelled in a straightforward way. This can make reading food ingredient labels difficult and it may be hard to know how a particular ingredient relates to your allergy.
Here are a few tips and things to keep in mind when reading a food label for food allergy:
Reading a food label for allergens is different from what you might be used to. It is more than just looking at the carbs, protein, salt and calorie count. Instead, for food allergies, the ingredient list and any warning labels are the most important. However, packaged and processed foods often contain many ingredients and sometimes they are not labelled in a straightforward way. This can make reading food ingredient labels difficult and it may be hard to know how a particular ingredient relates to your allergy.
Here are a few tips and things to keep in mind when reading a food label for food allergy: